Project Highlights
The Northern Border Region: A Health Focused Landscape
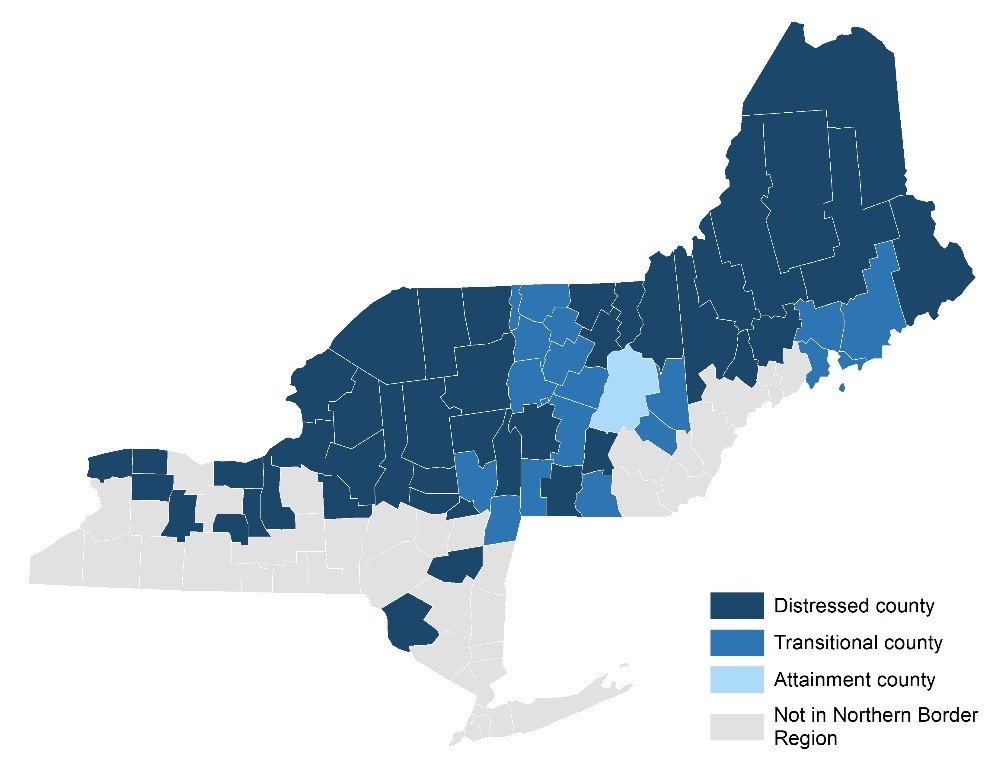
The Northern Border Regional Commission State and Region Chartbooks compile county- and state-level data related to health and health care access for the Northern Border Region and the individual states of Maine, New Hampshire, New York, and Vermont. Topics covered in the chartbooks include demographic and socioeconomic characteristics, access to care, health outcomes, mortality rates, Health Professional Shortage Areas, and the location of Rural Health Clinics, Federally Qualified Health Centers, hospitals, and substance use treatment facilities.
FMI: Katherine Ahrens, PhD (katherine.ahrens@maine.edu)
Webinar: Dr. Ahrens described this project which compiled the most recent publicly available data related to health and healthcare access at the county-level and state-level for the Northern Border Region: ME, NH, NY, and VT. Additionally, she discussed healthcare professional shortage areas and highlighted counties with worse health outcomes, as compared to the rest of the counties in the region.
Publications:

Ambulance Deserts: Addressing Geographic Disparities in the Provision of Ambulance Services
The declining numbers of rural hospitals and ambulance services imply that remaining ambulance services are being tasked to play a greater role in delivering emergency services in expanded service areas. Additionally, the delivery of ambulance services has not been systematically integrated, particularly in rural areas, leading to gaps in the provision of ambulance services, also known as “ambulance deserts.” To assist state and regional policymakers in formulating strategic plans to address these gaps, this project, led by Dr. Yvonne Jonk, aims to identify geographic disparities in accessing ambulance services by identifying and mapping ambulance deserts within each state, focusing on the following research questions:
- What areas of the states are ambulance deserts and how prevalent are they?
-
What percentage of each state’s population lives in an ambulance desert? Are there rural-urban or regional differences in the share of residents living in these deserts?
FMI: Yvonne Jonk, PhD (yvonne.jonk@maine.edu)
Chartbook released May 2023: Ambulance Deserts: Geographic Disparities in the Provision of Ambulance Services
CURRENT/ONGOING PROJECTS
Excess Deaths Associated with COVID-19 in Rural Communities
Quantifying excess deaths associated with the COVID-19 pandemic can provide a more complete measure of the total burden of the pandemic on mortality. While the National Center for Health Statistics maintains an online dashboard of US excess deaths associated with the COVID-19 pandemic overall and by race/ethnicity and age, excess deaths by rurality of residence are not tabulated and we aim to fill that gap. This project is completed and a journal article has been published in the Journal of Rural Health (early release Dec. 11, 2023). Ahrens KA, Rossen LM, Milkowski C, Gelsinger C, Ziller E. Excess deaths associated with COVID-19 by rurality and demographic factors in the United States. J Rural Health. Published online December 11, 2023. doi:10.1111/jrh.12815
FMI: Kate Ahrens, PhD, katherine.ahrens@maine.edu
Health Care Use and Access Among Rural & Urban Elderly Medicare Beneficiaries
Elderly individuals age 65 and over constitute the majority of the Medicare population, and among Medicare beneficiaries, health care access problems are greater among individuals with low incomes, in poor health, and with four or more chronic conditions. These and other barriers may lead to rural-urban differences in health care use among the elderly. This study uses the 2011-2013 Medicare Current Beneficiary Survey to compare health access and use of health services among fee-for-service Medicare beneficiaries age 65 and over in rural versus urban settings, and the factors associated with rural access problems. Findings from this study will help policymakers understand the needs of the growing elderly population and how best to adjust Medicare benefit design and service delivery to reduce barriers to care.
FMI: Yvonne Jonk, PhD
Health Care Use and Expenditures among Rural and Urban Medicare Beneficiaries Aged 85 and Over
The proportion of U.S. residents aged 85+ is expected to grow substantially in the coming decades with the impact of this growth in rural areas likely to be particularly pronounced. In light of this population’s significant health and other vulnerabilities and high costs, this project will use data from the Medicare Current Beneficiary Survey (MCBS) to examine rural-urban differences in health care use and expenditures among Medicare enrollees aged 85 and over.
FMI: Yvonne Jonk, PhD
How are Rural Health Clinics Serving Pediatric and Obstetrical Medicaid Populations?
This mixed methods study will examine the extent to which independent and provider-based services are serving pediatric and obstetrical patients covered by state Medicaid Programs. Using Medicaid Claims and brief qualitative interviews with 9 to 12 RHCs that specifically provide pediatric or obstetrical patient services, we will address the following research questions:
-
To what extent are RHCs providing pediatric and obstetrical services to patients enrolled in state Medicaid programs? Are there variations across states?
-
What diagnoses are most common for Medicaid pediatric and obstetrical patients using RHCs?
-
Are there differences in the extent to which provider-based and independent RHCs serve Medicaid pediatric and obstetrical services? Are there differences across the rural continuum and/or census regions? Are there differences in the extent to which RHCs serve pediatric and obstetrical services in Medicaid expansion vs. non-expansion states?
-
What are the Medicaid rates and reimbursement and coverage policies for pediatric and obstetrical services provided by RHCs?
-
What are the challenges and operational considerations encountered by RHCs providing pediatric and obstetrical services?
FMI: John Gale
Out-of-Pocket Spending Among Privately Insured Rural and Urban Residents
Out-of-pocket spending for health care services has been on the rise as deductibles and other cost-sharing requirements among the privately insured increase. This quantitative, nationally representative study will use the Medical Expenditure Panel Survey (MEPS) to examine health plan characteristics and out-of-pocket health care spending by non-elderly, community dwelling, rural and urban residents. Using bivariate and multivariable analyses, we propose to examine the:
- characteristics of private health insurance plans held by rural versus urban residents
- out-of-pocket costs, total premium and spending for privately insured rural versus urban residents
- percentage of health care spending paid out-of-pocket by rural versus urban residents and whether there are differences in out-of-pocket spending for individuals with chronic or acute health conditions, by events or socioeconomic characteristics?
- differences in out-of-pocket spending by plan characteristics
- percentage of rural versus urban household income represented by out-of-pocket health care spending, and whether this varies by socioeconomic and health plan characteristics
FMI: Erika Ziller, PhD
Prevalence of Opioid Prescribing, Diagnoses of Opioid Use Disorder, Treatment Patterns, and Costs Among Rural Medicare Beneficiaries
The elderly are at serious risk for opioid dependence or other harms due to higher prescribing patterns. However, there is a lack of literature on the rural-urban difference in the use and misuse of prescription opioids. Understanding these differences will help rural areas better target prevention and treatment options. We will address opioid prescribing rates among Medicare beneficiaries, using the Medicare Current Beneficiary Survey and describe differences in socioeconomic, health, and functional status of beneficiaries using prescription opioids and the general population using bivariate and logistic regression analyses. The impact of opioid use and medication-assisted therapy on health services utilization and costs will be assessed using difference in differences models.
FMI: Yvonne Jonk, PhD
Psychiatric Bed Closures in Rural Hospitals: An Assessment of Trends, Impact, and Policy Strategies
The closure of psychiatric beds in rural hospitals increases the wait time for mental health care and forces correctional facilities as well as hospital emergency departments, skilled nursing facilities, nursing facilities, and other health care providers to bear the burden of housing these patients until services become available. This study will examine trends in the closure of psychiatric beds by rural hospitals using the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Services Locator, the American Hospital Association (AHA) Annual Survey of Hospitals (2010-2017), and the Area Health Resources File.
FMI: John Gale, MS
Public Health Insurance Coverage among Rural and Urban Children
In recent decades, Medicaid and the Children’s Health Insurance Program (CHIP) have represented important sources of health insurance coverage for children, particularly those who live in rural areas. However, data suggest that the number of U.S. children covered by these public insurance sources has declined in recent years. Between 2016 and 2019, rates of public coverage among children declined slightly (39.5% to 37.1%) while the number of uninsured children increased by nearly 700 thousand. Some have speculated that changes in state health policy, particularly Medicaid eligibility shifts, have played a role in this coverage decline. However, it is unclear whether rural versus urban children have experienced comparable rates of decline or whether there have been geographic differences (by rurality or region) or disparities among specific rural populations. This study will address that gap using the Census Bureau’s American Communities Survey (ACS). Specifically, we will examine what percentage of rural and urban children was covered by Medicaid/CHIP in 2016-2020 versus 2011-2015 and whether any observed changes differ by rural-urban residence. We will also estimate who are the children eligible but unenrolled in Medicaid/CHIP and whether there are there rural-urban differences.
FMI: Erika Ziller, PhD, erika.ziller@maine.edu
Rural Health Access: Affordability and Barriers to Care
While the Affordable Care Act (ACA) led to pronounced gains in insurance coverage in rural areas, particularly among low-income individuals, rural residents continue to have higher rates of uninsurance than their urban counterparts. Research also suggests that paying for health care remains a substantial rural concern: A recent survey of rural adults identified financial challenges, followed by health and health care issues, as the most pressing problems facing rural families, with many citing affordability as the reason for delaying or foregoing needed care. Although we know that health care affordability remains a concern for many rural residents, it is unclear to what extent factors such as insurance coverage gains or the growing trend of high deductible health plans (HDHPs) have influenced rural experiences of cost-related barriers to care, and whether rural populations continue to experience more such barriers than do urban residents. This quantitative, nationally representative study will address this research gap by comparing rural and urban differences in health care access and affordability.
FMI: Erika Ziller, PhD, erika.ziller@maine.edu
Rural Poverty and Health: A Chartbook
Using the Medical Expenditure Panel Survey (MEPS), The National Health Interview Survey (NHIS), and the National Survey of Drug Use and Health (NSDUH), we will examine relationships between poverty and health for community-dwelling rural and urban residents of all ages. Analysis of county-level health-related measures using the County Health Rankings will supplement the national survey data. We will produce a chartbook that addresses the following research questions:
- Among rural residents, do individuals who are poor, or near-poor differ from their non-poor counterparts with respect to health status, health care access and use, risk/protective factors, and physical environment?
- Among individuals who are poor or near-poor, are there rural-urban differences on the health-related measures of interest (mentioned above)?
- Are rural-urban differences on health-related measures greater among individuals who are poor or near-poor than among those who are non-poor?
- What additional factors are associated with rural poverty and health, and do relationships between these factors and poverty differ across rural and urban contexts?
- What are the health-related characteristics of rural counties with high rates of poverty and persistent poverty? How do these counties compare to non-poor rural counties and poor urban counties on health-related metrics?
FMI: Jean Talbot, PhD
Rural-Urban Differences in Out-of-Pocket Prescription Drug Spending
This study will use the Medical Expenditure Panel Survey to examine out-of-pocket spending on prescription medication from 2014-2017. Specifically, we propose to analyze total spending and out-of-pocket spending for rural versus urban residents. We will identify the percentage of prescription drug spending that is paid out-of-pocket by rural and urban residents—across all drugs and within certain drug classes of interest (e.g., medications for diabetes, behavioral health conditions, asthma, and cancer). We will also examine how rural and urban out-of-pocket spending for prescription drugs differ based on health insurance coverage and other socioeconomic variables.
FMI: Erika Ziller, PhD
Socioeconomic Profiles and Market Characteristics Associated with Ambulance Deserts
This project builds on our recent work identifying areas across the country lacking adequate access to ambulance services (i.e., ambulance deserts). Because these areas are newly identified, little is known of the populations living in ambulance deserts or of the market characteristics associated with ambulance deserts. Factors contributing to ambulance deserts include:
- Declining number of rural hospitals and ambulance services
- Lack of integration of ambulance services into the rural healthcare system
- Gaps in the provision of rural ambulance services, increasing the geographic coverage areas for existing ambulance services.
To assist state and regional policymakers in formulating strategic plans to address these gaps we will use our existing ambulance and ambulance desert location data and data from the U.S. Census to identify vulnerable populations living within ambulance deserts and the implications associated with traveling to the nearest health care facility capable of serving the emergent healthcare needs of these vulnerable populations.
FMI: Yvonne Jonk, PhD, yvonne.jonk@maine.edu
Understanding Rural Health Clinic Services, Use, and Reimbursement
This study will use Medicare claims data to describe the scope and intensity of services provided to Medicare beneficiaries by independent and provider-based Rural Health Clinics (RHC)s. This study will address the following research questions:
- What are the most common diagnoses for Medicare beneficiaries using RHCs?
- What are the characteristics and intensity of the services (e.g. E&M services, other procedures) provided by RHCs?
- Are there differences in the intensity and type of clinical services provided by different types of RHCs (i.e. provider-based vs. independent) and across the rural continuum and/or census divisions/regions?
- What types of non-RHC services are RHCs billing to Medicare Part B (e.g. care management, telehealth, inpatient E&M services, other procedures)?
- How do estimated fee for service payments to RHCs under CMS’s changes to the outpatient E&M codes in 2021 compare to the 2021 per-visit reimbursement cap?
FMI: John Gale, MS
Understanding Rural Non-Emergent Emergency Department Use
Research indicates that rural residents use the emergency department (ED) at higher rates than their urban counterparts, with recent analyses indicating that this rural-urban difference has been increasing. Additional studies suggest that rural residents are more likely to visit the ED for a non-emergent reasons. However, the reasons for these higher rates remain unclear. This difference could be the result of rural primary care access barriers, including availability of after-hours care, or could be related to lower education or other factors affecting knowledge of appropriate healthcare use. This study will use the 2014-2017 Medical Expenditure Panel Survey to analyze the factors associated with rural versus urban residents’ non-emergent ED use.
FMI: Erika Ziller, PhD
Unmet Health and Social Needs of Rural Residents with Disability
There is growing evidence that a consequential percentage of individuals who become infected with COVID-19 will develop long-term health conditions, some of which may be disabling. Even before the public health emergency, disability was a substantial concern in the United States, affecting more than 61 million adults nationally. Prior research has confirmed that the prevalence of disability is particularly pronounced in rural communities and rural residents experience disability at higher rates than their urban counterparts. Some analyses have suggested that rural-urban disparities in disability prevalence are particularly pronounced among Black and other minoritized races and ethnicities. Extensive research suggests individuals with physical and mental disabilities may experience multiple barriers to needed healthcare and social supports. Although research is limited, poorer access to insurance coverage, lower rates of specialty care availability, and greater travel distances may place rural residents at greater risk for unmet needs, and some single-state and qualitative studies suggest that rural residents with disabilities struggle to obtain primary and specialty care because of affordability, availability, and transportation issues. However, the lack of national data on rural-urban differences in access to healthcare services may limit policymakers’ abilities to develop comprehensive strategies to address any access concerns. This project will address this gap by examining rural-urban differences in access to health care and social wellbeing for adults experiencing disability.
FMI: Erika Ziller, PhD, erika.ziller@maine.edu
Use of Z codes by Rural and Urban Providers to Capture Data on the Social Determinants of Health Impacting Medicare Beneficiaries
There is wide recognition that social determinants of health (SDOH) are significant drivers of health risks and outcomes and account for more than 60 percent of an individual’s overall health. Recent research has recognized the importance of SDOH data and the necessity of collecting these data to empower providers to address health disparities. Despite this, the collection of SDOH data remains inconsistent. Z codes are a set of reason codes within the ICD-10-CM introduced in 2015 to capture data on SDOH impacting the health of patients. Previous studies have documented higher rates of the top five chronic conditions (hypertension, depression, hyperlipidemia, rheumatoid arthritis, and chronic kidney disease) among Medicare fee-for-service (FFS) beneficiaries with reported Z codes compared to all Medicare FFS beneficiaries. Research has found use of Z codes to be low.
We will examine 2019-2021 Medicare inpatient, outpatient, and carrier claims data to evaluate the use of Z codes by rural and urban providers to capture information on SDOHs affecting the health of rural Medicare FFS beneficiaries by age, gender, and rural residence across the rural continuum. We will interview key provider types from critical access hospitals and other rural and urban hospitals, rural health clinics, and federally qualified health clinics to understand opportunities to improve the use of Z codes by these providers.
FMI: John Gale, MS, john.gale@maine.edu and Kate Ahren, PhD, katherine.ahrens@maine.edu
COMPLETED PROJECTS
A Current Examination of HIV and Hepatitis C in Rural Counties
Rural counties have witnessed significant growth in opioid pain reliever misuse and initiation of injection drug use. As a result, human immunodeficiency virus (HIV) prevalence, acute hepatitis C virus (HCV) incidence, and maternal HCV infection have grown among certain rural subpopulations over the past decade. Establishing current, county-level HIV prevalence and acute HCV incidence estimates across the rural-urban continuum could inform policies and practices aimed at addressing the transmission and treatment of HIV and HCV in rural areas. Using existing data from federal and state sources, we produced a chartbook on county-level data on HIV prevalence and acute HCV incidence, and examined the availability of Ryan White HIV/AIDS medical providers and other HIV and HCV treatment and testing services across the rural-urban continuum. Our findings showed that HIV prevalence for rural counties was highest in southern states; but within these states, rates were higher in urban counties than rural. We also found lower availability of Ryan White providers in rural compared with urban counties. Using data from the U.S. natality files, our associated peer-reviewed article examines rural-urban differences in county-level rates of maternal infection with hepatitis C virus (HCV) during 2010-2018. Findings can help inform implementation of community-level interventions to reduce maternal HCV infection and narrow rural-urban disparities. Completed publications:
- Rural HIV Prevalence and Service Availability in the United States: A Chartbook
- Rural-Urban Residence and Maternal Hepatitis C Infection, United States: 2010-2018
- Webinar presented April 21, 2017
FMI: Katherine Ahrens, PhD or Amanda Burgess, MPPM, MPH
Access to Mental Health Services and Family Burden of Rural Children with Significant Mental Health Problems
Access to and Use of Home and Community-Based Services in Rural Areas.
Acuity Differences Among Newly Admitted Rural and Urban Nursing Home Residents
Building on studies showing differences in how rural and urban older adults access and use long-term services and supports (LTSS), this study will use national, standardized Medicare and non-Medicare nursing home assessment data (MDS 3.0) to to assess rural-urban acuity differences among newly-admitted older nursing home residents. Study findings will inform federal and state policy strategies to enable rural (and urban) older adults to access LTSS services most appropriate to their social, health, and functional needs. This study is complete and findings were published in The Gerontologist (doi:10.1093/geront/gnaa183).
FMI: Yvonne Jonk, PhD, yvonne.jonk@maine.edu
Adolescent Alcohol Use in Rural Areas: What are the Issues?
Adverse Childhood Experiences (ACEs) and the Health Status of Rural Residents.
Ambulance Deserts: Addressing Geographic Disparities in the Provision of Ambulance Services
Declining numbers of rural hospitals and ambulance services imply that remaining ambulance services are being tasked to play a greater role in delivering more sophisticated emergency services in expanded service areas, yet EMS has not been systematically integrated within the healthcare delivery system. Research has shown that this lack of systems planning has led to gaps in the provision of ambulance services, exacerbated across larger geographic coverage areas. These gaps—referred to as “ambulance deserts”—are steadily increasing. To assist state and regional policymakers in formulating strategic plans to address these gaps, this 2-year project will employ a systematic methodology within a geographic information system (GIS) framework for identifying the adequacy of the existing sets of ambulance services (by state) to meet the needs of the communities they serve, and the extent to which states have populated areas that are not served by any ambulances. Year one activities will focus on building a database of ambulance service locations, which will be followed up in year two with identifying and creating maps of ambulance deserts within each of the selected study states. A chartbook was released in May 2023.
FMI: Yvonne Jonk, PhD, yvonne.jonk@maine.edu
Assessing Health Information Technology (HIT) Strategies to Improve Access for Rural Veterans
Assessing HIT Readiness of Rural Health Clinics: A National Survey.
Capacity of Rural Counties to Respond to an HIV or Hepatitis C Outbreak
Rural counties may be potentially vulnerable to an HIV or hepatitis C outbreak among persons who inject drugs. Using mixed methods, we provide an understanding of the rural areas at risk of an outbreak based on their state and county characteristics and an assessment of their public health infrastructure. Completed publications:
- Capacity of Rural Counties to Address an HIV or Hepatitis C Outbreak
- Voices From the Field: A Qualitative Study of the Challenges and Promising Practices of Rural Public Health in Addressing HIV and Hepatitis C (Journal of Health and Human Services Administration, in press).
- Webinar presented April 12, 2017
FMI: Amanda Burgess, MPPM, MPH (amanda.burgess@maine.edu)
Catastrophic Consequences: The Rise of Opioid Abuse in Rural Communities.
Challenges and Opportunities for Improving Rural Long-Term Services and Supports: Integrated Care Management in Rural Communities
Challenges and Opportunities for Improving Rural Long-Term Services and Supports under the Affordable Care Act
Consequences of Rural Uninsurance
Developing a Sentinel Cohort of Rural Health Clinics for Use in Developing Relevant Quality Measures and Monitoring Program Performance.
Eligibility Transitions under the Affordable Care Act: Policy Considerations for Ensuring Coverage Continuity Among Rural Residents.
Expanded Look at Rural Access to Care.
Health Care Access and Affordability Among Rural Children with Public Versus Private Health Insurance.
Health Insurance Stability among Rural Children Following Public Coverage Expansions
Health Care Use and Access Among Rural & Urban Non-elderly Disabled Medicare Beneficiaries
FMI: Erika Ziller, PhD erika.ziller@maine.edu
Impact of Employment Transitions on Health Insurance Coverage of Rural Residents
Impact of the Opioid Crisis on Rural Emergency Departments
This study used data from the Nationwide Emergency Department Sample (NEDS) and information from a panel of rural emergency care experts to assess the impact of the opioid crisis on rural emergency departments (EDs). Findings will help inform policies designed to help rural health care systems and communities address the growing problem of opioid abuse. Completed publication:
FMI: Jean Talbot, PhD, MPH (jean.talbot@maine.edu) or Erika Ziller (erika.zillermaine.edu)
Implications of Mental Health Comorbidity and Rural Residence for Health Care Use Patterns of Individuals with Chronic Disease
Issues Related to Rural Health Clinic (RHC) Participation in CMS’s Merit-Based Incentive Payment System (MIPS).
Knowledge of Health Insurance Concepts and the Affordable Care Act among Rural Residents
Out-of-Pocket Costs Among Rural Medicare Beneficiaries
Patterns of Care for Rural and Urban Children with Mental Health Problems
Prevalence and Impact of High Deductible Health Insurance Plans in Rural Areas
Preventive Health Service Use Among Rural Beneficiaries.
Preventive health services and screenings are an important component in the continuum of care provided to individuals across all ages. Yet, research has shown that rural residents use fewer preventive health services and screenings.This study used the National Health Interview Survey to examine receipt of preventive health services (cholesterol check, fasting blood sugar test, mammogram, pap smear, and receipt of the HPV vaccine) by rural and urban women over the age of 18. Findings indicate that rural women were less likely than their urban peers to receive preventive health services, and that some of the differences may be explained by rural-urban differences in sociodemographic characteristics. However, even when controlling for these characteristics, lower use of mammogram or HPV vaccine among rural remained. Outreach efforts targeted to rural women, along with policies and programs designed to improve access to rural women’s cancer screening and HPV participation, are needed. A recent Research & Policy Brief has been published and is cited in the Rural Health Research Gateway’s April 2019 Research Recap: State of Women’s Healthcare Utilization and Health Indicators..
FMI: Erika Zilller, PhD
Provision of Specialty Mental Health Services by Rural Health Clinics
Role and Early Impact of CO-OPs in the Rural Health Insurance Marketplace.
Rural Demography and Aging: The LTSS Imperative in Rural America.
Rural E-Mental Health: Models That Enhance Access, Service Delivery, and Integration of Care
Rural Health Clinic Financial Performance and Productivity
This study used Medicare cost reports for independent and provider-based clinics to provide a detailed national picture of the financial and operational performance of Rural Health Clinics (RHCs) and described variations in performance related to revenue, costs, staffing, payer mix, productivity levels, and hours of operation across independent and provider-based clinics. The project is completed. The Research & Policy Brief examines the costs of RHCs relative to Medicare payment limits for different types and sizes of RHC providers.
To view or download the Research & Policy Brief, please visit: https://digitalcommons.usm.maine.edu/clinics/13/
FMI: John Gale, MS
Rural Health Clinics Chartbook
The Rural Health Clinic (RHC) Program, established in December 1977 by the Rural Health Clinic Services Act, P.L. 95-210, is one of the nation’s oldest rural health support programs. RHCs were developed to address geographic primary care access barriers experienced by Medicare and Medicaid populations living in rural underserved areas. RHCs are an important source of primary care services in rural areas with 4,888 RHCs serving the residents of 45 states as of September 2021, and have come to be recognized for their role in serving vulnerable rural populations.
Community Characteristics and Financial and Operational Performance of Rural Health Clinics in the United States: A Chartbook builds on our extensive body of work on RHCs and our 2003 RHC Chartbook providing an overview of Rural Health Clinic (RHC) characteristics and issues using data from CMS’s Provider of Services file, Medicare Cost Reports, and the Robert Wood Johnson Foundation’s’ County Health Ranking. The Chartbook provides a discussion of the challenges related to collection and reporting of RHC quality data and will be useful to policymakers and others interested in the performance of RHCs nationally. It can also be useful to RHC administrators to benchmark staffing patterns, productivity, and efficiency.
FMI: John Gale, MS (john.gale@maine.edu)
Rural Maternal Smoking Behaviors
Rural Mental Health First Aid Evaluation.
Rural Residential Care: The Implications of Federal and State Policy
Safety Net Activities of Independent Rural Health Clinics
Tobacco Treatment in Rural Primary Care
Tobacco use is related to 440,000 deaths each year, making it the leading cause of preventable death and disease in the U.S. Though tobacco use declined from 43% in 1965 to 18% in 2014 among the general U.S. population, tobacco use remains high among several vulnerable subpopulations, in particular, residents of rural areas. Primary care is an important resource in tobacco prevention, but little is known about the degree to which rural primary care providers counsel or prescribe medications for smoking cessation. Using data from the National Ambulatory Medical Care Survey, we compared rural and urban rates and predictors of tobacco counseling and treatment medication prescribing by primary care providers.
This study was published in the Journal of Rural Health and compares the performance of rural and urban primary care providers in adhering to evidence-based smoking-related standards of care and assesses the degree to which electronic health record use was related to improved adherence to these standards in the practice of rural versus urban providers.
Talbot, J. A., Ziller, E. C., & Milkowski, C. M. (2021, September). Use of Electronic Health Records to Manage Tobacco Screening and Treatment in Rural Primary Care. Journal of Rural Health, online. https://doi.org/10.1111/jrh.12613
Transformation of Rural Health Clinics: Are They Ready to Service as Patient-Centered Medical Homes?
Understanding Differences in Rural and Urban Adolescent and Young Adult Substance Use.
Recent research suggests that rates of adolescent alcohol, tobacco, and illicit drug use are on the decline. Early results from the 2016 Monitoring the Future annual survey show a continued long-term decline in adolescent substance use across marijuana, alcohol, tobacco, and misuse of some drescription medications. This project examines rural-urban differences in substance use among adolescents and young adults using data from the 2008-10 and 2014-16 National Survey on Drug Use and Health. Early findings revealed large rural-urban differences in cigarette use by adolescents so our first set of analyses examined change in cigarette use over time, and we presented these findings in a poster at the 2018 National Rural Health Association meeting, and published an article in the American Journal of Public Health.
FMI: Erika Ziller, PhD